KIDS BROKEN ARM
PEDIATRIC PROXIMAL HUMERUS FRACTURE
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently.
related talks: broken forearm (green stick fracture), broken elbow (supracondylar fracture), broken wrist; broken inner elbow (medial epicondyle fracture); broken outer elbow (radial head fracture, or lateral condyle fracture).
What is a Broken Arm (Pediatric Humerus Fracture)?
A broken arm is a very common injury in kids. The break can occur anywhere along the arm. The most common sites are the wrist (see talk), the forearm (see talk), the elbow (see talk), and the upper arm...near the shoulder.
This talk will discuss injuries to the upper arm (which involves the Humerus bone).
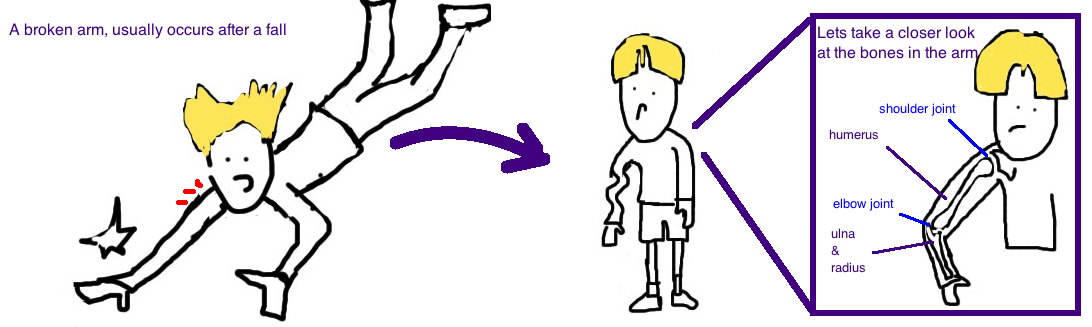
Lets quickly review the anatomy of the arm. The shoulder joint is where the arm bone (humerus) meets up with the shoulder blade (scapula) and the collar bone (clavicle). The elbow joint is where the arm bone (humerus) meeds up with the two bones of the forearm (the radius bone and the ulna bone). The humerus bone is softest at the ends, and most commonly breaks near the shoulder (called a proximal humerus fracture) or near the elbow (called a supracondylar elbow fracture). Kids usually break their arm after falling off the monkeybars or after falling onto an outstretched arm.
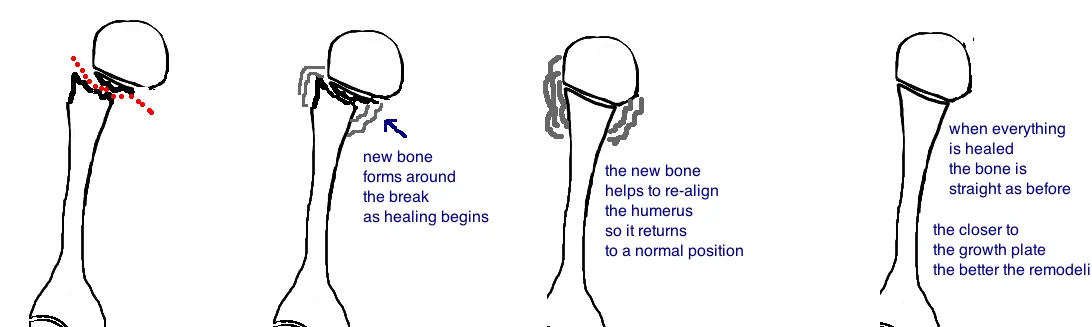
Because kids are still growing, most broken bones heal very well, and the arm bone is no exception. The younger the child, the better their broken arm will heal.So why do kids heal so well? Its because a kid's bones are actively growing (in an "anabolic state"), so filling in a small crack isnt a big deal when its expanding a few centimeters a year anyway.
As kids, we get taller because our bones get longer. Bones get longer because of growth plates located at the ends of each bone, and these growth plates slowly create new bone, first by making cartilage, and then this new cartilage gets calcified.
Like all the other bones in our arms and legs, the humerus bone has a growth plate at each end (one near the shoulder and one near the elbow), however they don't contribute equally to the growth of the arm bone... 80% the growth comes from the "proximal growth plate" (the one near the shoulder). This is important when talking about a broken arm. A crack that occurs near a growth plate heals very quickly because the bone is already being made so actively. Also, if the bone not only breaks, but also moves out of alignment, the bone somehow knows that it should be straight, and it will re-align itself in a process called "remodeling". The remodeling potential of a bone is greatest near an active growth plate.
Diagnosis of a Broken Arm (Pediatric Humerus Fracture):
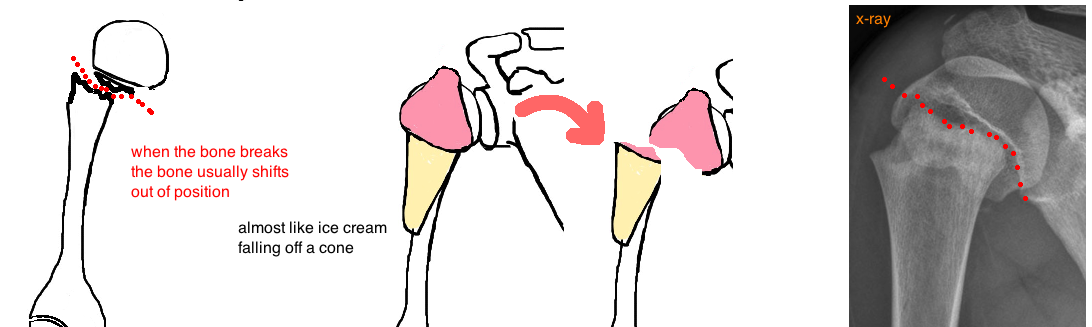
Kids usually report falling onto their arm and then feeling significant pain and inability to use the injured arm. Sometimes there is an obvious deformity (the arm is bent out of place).
A doctor that is suspicious for a broken arm will order x-rays. X-rays are great for showing the break and helping doctors decide how to treat the injury.
A broken arm is not just a "yes" or "no" diagnosis (doctors look for more information on an x-ray besides seeing if there is a crack in the bone). They also look at x-rays to make sure the shoulder is not dislocated, they look to see how much mal-alignment of the arm bone was caused by the break, and they look to see how much growth the child has left. Doctors also examine the child to make sure the nerves and arteries are working well after the injury, and also to make sure nothing else was injured (sometimes we pay so much attention to the major injury that we can completely ignore smaller, but important minor injuries like a broken finger or a big cut).
Treatment of a Broken Arm (Pediatric Humerus Fracture):
In general, fractures of the arm heal well with time and rarely require surgery. But a lot depends on the age of the child and the location of the break. In general, the younger the child, the better the bone will heal because they have more time to grow out of the injury (with time the broken bone doesnt just heal, but the bone actually straightens out on its own...incredible!).
The proximal humerus (the region of the arm bone nearest to the shoulder) has excellent "remodeling" potential because the growth plate here contributes 80% of growth to the arm. This means that surgery is rarely needed to help out with healing (bones with less remodeling potential, like every bone in adults, often requires surgery to re-align the break. Kids dont need any help). Kids less than 6 years old only need a sling to protect the arm while it heals (no matter how displaced the fracture).
As kids get older, their bones become more like adults and they start to lose the ability to remodel. Adolescents can still tolerate a significant mal-alignment with the potential to remodel, up to about 45° of angulation, or 50% contact between the two bones.
Beyond that point a surgeon usually needs to intervene because there is the risk of a lasting deformity (it will never become completely straight). Often times, the bone is re-aligned by the doctor while the child is sedated, and will then be placed into a sling, and will be followed every week with x-rays to ensure its healing well and hasnt slipped out of position. Sometimes the break is unstable, and even when its re-aligned, it will slip out of position again. In such cases surgery should be performed to hold the bone in good alignment using pins that are inserted through the skin into the broken bone and then removed 3-6 weeks later.
In contrast to fractures of the proximal humerus, fractures of the mid-humerus (mid-shaft fractures) have less remodeling potential because they are farther away from the growth plate. As a result, the body is less tolerant of deformity, less able to correct fractures that cause the bone to angulate. Compared to angulation of up to 80° in kids under 6 years old and angulation up to 45° in adolescents, a shaft fracture will only heal well if the angle is under 30°, which is still rather bent (so this part of the bone still has very good remodeling potential).
If there is deformity over 30°, kids may require surgery to straighten the bone, which is performed with a small plate and screws on the side of the bone, or a small nail that goes down the center of the bone.
What is the long term outcome?
There is occasionally a lasting bend in the arm after healing has completed. This usually doesnt correlate with any problems with arm function because the shoulder has so much motion that kids can compensate for any small abnormal angulation.
The biggest concern with a midshaft humerus fracture is injury to the radial nerve, which runs right along the bone starting at the middle side of the arm about 22 cm from the elbow, and travels against the bone for about 7 cm. If the break occurs at this same interval, there is a high risk for injury of the nerve. Symptoms of nerve injury include decreased sensation along the back of the forearm and hand, as well as muscle weakness in extending the wrist (see nerve damage talk).
The good news is that these injuries are usually temporary, and will correct over the course of 3 months. Often times the nerve is over stretched when the bone is injured (almost how you strain a ligament), which is called neuropraxia, and needs a few weeks to heal completely without long term deficits. Sometimes the nerve can get caught within the bone fragment, and will heal as the bone repairs, without need for surgery. If the nerve has still not returned to normal at 3 months, surgery is indicated to explore where the nerve is injured. The radial nerve is a strong nerve and has the ability to heal months after injury.
DID WE ANSWER YOUR QUESTIONS? IF NOT, PLEASE EMAIL US: contact@bonetalks.com
Reference
1) Pahlavan S et al. Proximal humerus fractures in the pediatric population: a systematic review. J Child Ortho. 2011; 5:187-94. full article.
2) Dobbs MB et al. Severely displaced proximal humeral epiphyseal fractures. J Ped Ortho 2003; 23: 208-215. full article. good surgical outcomes.
3) Hutchinson PH, Bae DS, Waters PM. Intramedullary nailing versus percutaneous pin fixation of pediatric proximal humerus fractures: a comparison of complications and early radiographic results. J Ped Ortho 2011; 31: 617-22. full article. both have pros and cons.
4) Neer CS, Horowitz BS. Fractures of the proximal humeral epiphysial plate. CORR 1965; 41: 24-31. full article. classic promoting nonop.
5) Bahrs C et al. Proximal humeral fractures in children and adolescents. J Ped Ortho 2009; 29; 238-42. full article. nonop does well, if surgery req. then outcome is also good.
6) Burgos-Flores J et al. Fractures of the proximal humeral epiphysis. Int Ortho 1993; 17: 16-19. full article. outcome depends on age, consider op for older kids.