BROKEN KNEE
(TIBIAL PLATEAU FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
related talks: kneecap dislocation; broken kneecap, runners knee
What is a Broken Knee (Tibial Plateau Fracture) ?
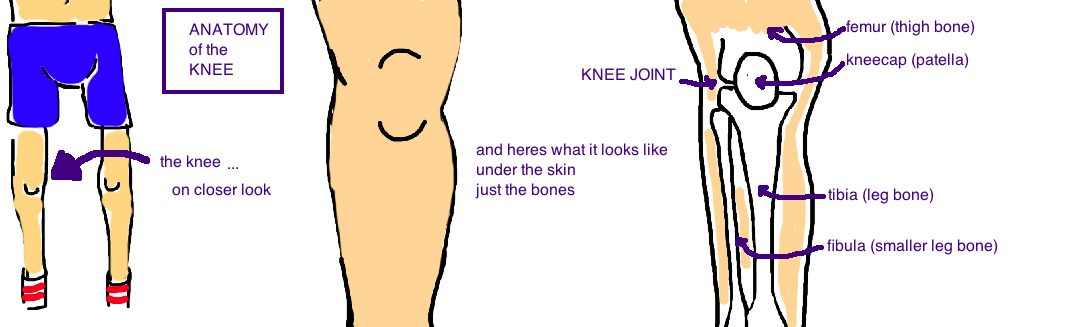
The technical name for a broken knee is a "Tibial Plateau Fracture", which is a break along the joint surface of the knee (but really its a break in the tibia bone, aka "shin bone"). It can be thought of as a broken knee because the main concern in treating this injury is the preservation of the knee's cartilage.
To better understand this injury, lets first review the anatomy of our knee.
The knee joint is where the leg bone (tibia) joins with the thigh bone (femur). The knee has two compartments, an inside (medial) and a outside side (lateral) compartment (also known as the medial and lateral tibia condyle).
The tibial plateau fracture can occur on the lateral side (most common), the medial side, or both.
The break occurs when a strong force bends the knee inward or outward causing a force that breaks the tibia bone. This excessive force can either 1) split, 2) squish ("compress"), or 3) both split and squish the tibia bone.
Because the mechanism of injury is a powerful bending force, the ligaments along the sides of the knee that normally provide stability are commonly torn. In younger people, the injury only occurs after a lot of force (it a takes a big accident to break this bone), and therefore its usually seen in combination with ligament injuries.
The meniscus is located within the knee and its closely attached to the tibia joint surface, so this too is commonly torn (see talk) in combination with tibial plateau fractures.
In elderly people, the tibia bone can weaken from osteoporosis (a condition of thinning bone that occurs in varying degrees to all of us as we age) and therefore a tibia plateau fracture may occur after a simple fall from standing height. In these cases its unlikely that other structures of the knee (like the meniscus or ligaments) are injured because this break occurred due to weak bone not because there was a high-energy injury.
Diagnosing a Broken Knee (Tibial Plateau Fracture):
A tibial plateau fracture will cause significant knee pain and swelling. People will be unable to stand on the leg due to pain.
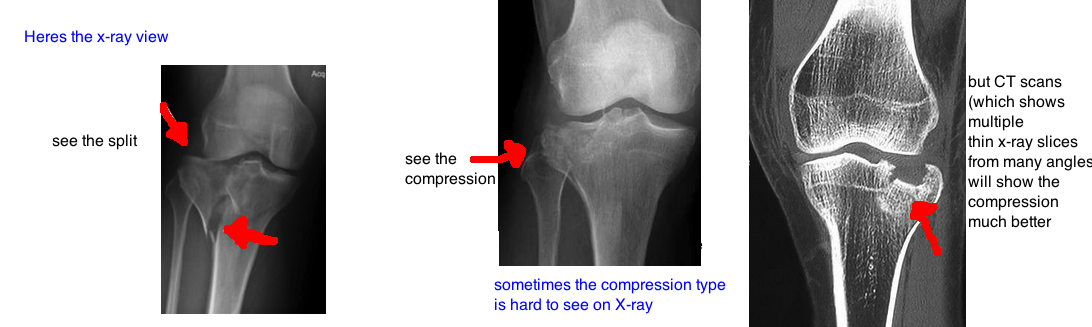
Doctors concerned for a break will order X-rays that provide the diagnosis, and also tell doctors how severe the injury is.
In cases of a simple fracture pattern, the x-rays give enough information to plan the treatment. In cases where the tibia plateau looks broken in multiple places, a CAT scan (which provides 3D x-ray images) gives extra information that is helpful for treatment (this usually means surgical planning). In fact, one study showed that CAT scans are so good at showing the details of the break, that it changes the way doctors will treat in the injury in about 25% of cases.
Its important to not only diagnose the fracture, but also to identify other knee injuries if the fracture occurred from a car accident or other high-energy injury. Examination is often limited by pain, but the doctor will test the side to side stability of the knee to look for collateral ligament injury, or ACL/PCL tears, or meniscus tears.
Treating a Broken Knee (Tibial Plateau Fracture):
Treatment depends on the severity of injury. The goal is to prevent a knee deformity, to enable normal knee motion, and to minimize the risk for future post-traumatic arthritis that causes knee pain.
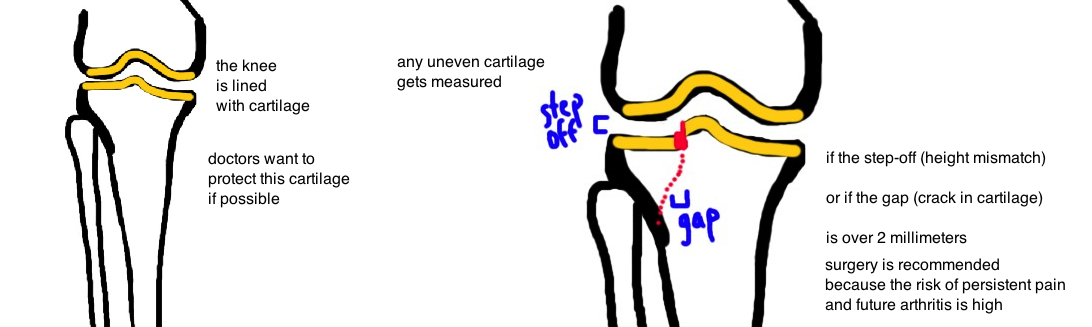
The knee joint is lined with cartilage (this means there is a layer of cartilage sitting at the end of both the femur and the tibia bone, which provides a smooth surface while your knee bends). This surface needs to remain smooth and level otherwise too much friction will occur and the cartilage will be prematurely destroyed (its like trying to drive on a smooth road versus a road lined with pot holes: the bumpy road will be painful can cause the car to break down). In knees, the same applies, and an uneven joint surface will cause pre-mature Knee Arthritis (see talk).
The problem is that doctors still don't know how bumpy this surface is allowed to be before surgery is required to fix the knee (fill in the pot holes to use the road analogy).
Some of it depends on where the break (or "bumps") occur within the knee, how old the person is, and how high-energy the initial force was that caused the break.
While historically some doctors say up to 10 mm of uneven terrain is ok, most doctors currently believe about 3 mm or less is acceptable (the knee is surprisingly resilient, other joints in the body can only tolerate less than 2 mm of unevenness without having a high risk for early arthritis).
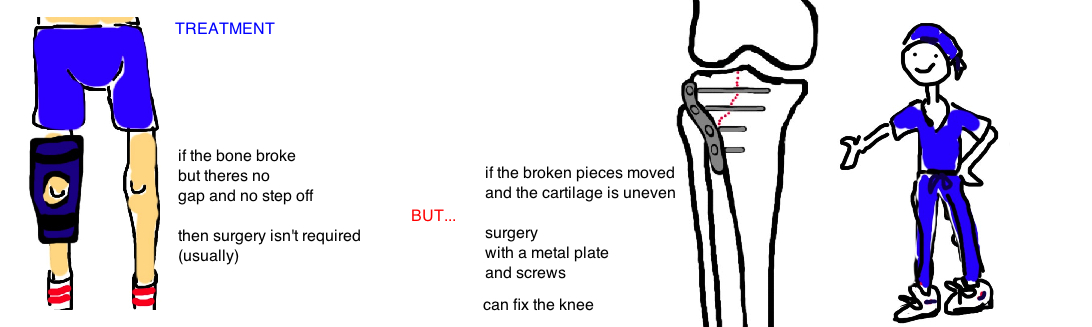
So surgery isn’t required in all cases.
A hairline crack, or a mild compression of the bone will heal well with a hinged-knee brace (to allow for knee motion during rehabilitation), and a few weeks without putting weight on the affected leg. As long as all of the goals of treatment (normal knee motion, minimal arthritis risk) can be satisfied, a person will be very fortunate to heal without the pain and risk of infection that comes with any surgery.
But surgery is commonly needed for high-energy breaks which cause significant joint line incongruity (unevenness), multiple breaks, and ligament injury.
The big problem with these injuries is that the normal architecture of the knee is destroyed so when all the dust settles, the knee is out of alignment and feels unstable to people. The proceeding knee instability is the biggest risk factor for future disability and arthritis.
So what does surgery involve?
In a split fracture, doctors will use a metal plate and screws to push the bone fragments back together. In a compression fracture, the squished bone may need to be reinforced with bone-like material (freeze dried calcium, they kind of look like bread crumbs) in addition to getting a metal plate and screws.
After surgery the bone needs time to heal, and people will be advised to keep off the leg for 6-8 weeks until the bone is strong enough to bear your body weight again.
In cases of very high-energy trauma, the soft tissue (muscle, fat, skin) surrounding the fracture might be too damaged to withstand the extra stress of a surgery (remember that surgery involves a knife). In such cases, pins are placed into the bone and the knee is held in place with a metal frame on the outside of the leg (called external fixation, or medical slang “ex-fix”) which stabilizes the knee until the soft tissue has time to heal. In a week or two, once the swelling has improved and the tissue surrounding the bone is happier, the above mentioned surgery is performed to fix the break.
What is the long term outcome?
The long-term outcome really depends on how high-energy the initial injury was. The bone will typically heal well once surgically repaired, but the cartilage is a different story. Cartilage doesn’t heal very well (that’s why we cant turn back the clock with arthritis, and the mainstay of treatment is a joint replacement).
Surgery will minimize future damage to the cartilage but it cannot undo damage from the initial impact. Surgery will also restore general knee alignment so that people feel stable on their leg. Stability has been shown to be the most important thing to restore with surgery to provide the best outcome.
References
1) Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Ortho Trauma. 1987; 1: 97-119. full article.
2) Chan et al. Impact of CT scan on treatment plan and fracture classification of tibial plateau fractures. J Ortho Trauma 1997; 11: 484-9. full article. ct scans affect treatment decision: 58% to 71% operative. changed surgical plan 25%.
3) Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Ortho Rev. 1994; 23: 149-54. full article. anatomic reduction causes high tissue complication.
4) Weigel DP, Marsh JL. High-energy fractures of the tibial plateau. Knee function after longer follow-up. JBJS 2002; 84: 1541-51. full article. knee arthritis ok with 3 mm step off.
5) Porter BB. Crush fractures of the lateral tibial table. Factors influencing the prognosis. JBJS Br 1970; 52: 676-87. full article. 1 cm step off threshold for treatment.
6) Lansinger O et al. Tibial condylar fractures. A twenty-year follow-up. JBJS 1986; 68: 13-19. full article. knee stability in extension is key.
7) Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968-1975. CORR 1979; 138: 94-104. full article. classic paper.
8) Berkson EM, Virkus WW. High-energy tibial plateau fractures. JAAOS 2006; 14: 20-31. full article. incidence of arthrosis depends on instability: valgus >10 deg 80%, vs. only 14% if <10 deg.
Questions? Email us: contact@bonetalks.com