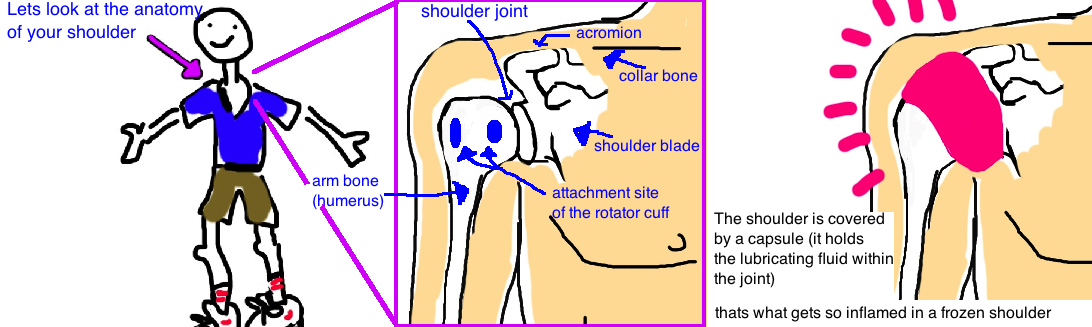
ADHESIVE CAPSULITIS
"FROZEN SHOULDER"
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
related talks: rotator cuff tear; biceps tendon tear; biceps tendonitis; SLAP tear; shoulder arthritis; rotator cuff arthritis