BROKEN LEG
(TIBIAL SHAFT FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor or call 911. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
What is a Broken Leg (Tibia Shaft Fracture)?
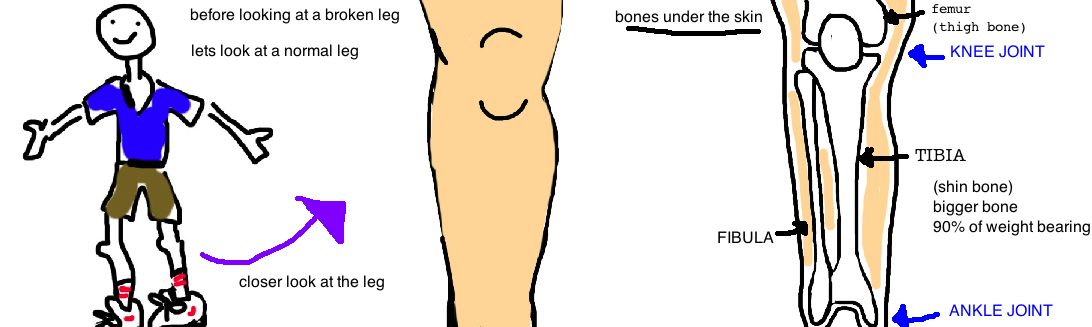
Your classic Broken Leg is most commonly an injury to the Tibia bone (the injury is also called a Tibial Shaft Fracture).
The leg (below your knee) has two bones the Tibia and the Fibula, however the Tibia is the larger bone and bears about 90% of the body weight.
Tibia fractures can occur 1) at the knee joint, and are called “Tibial Plateau Fractures” (see talk) or they can occur 2) around the middle of the tibia (called "Tibial Shaft Fractures", thats what this talk is about) or they can occur 3) near the ankle joint, and these are called “Pilon Fractures” (see talk).
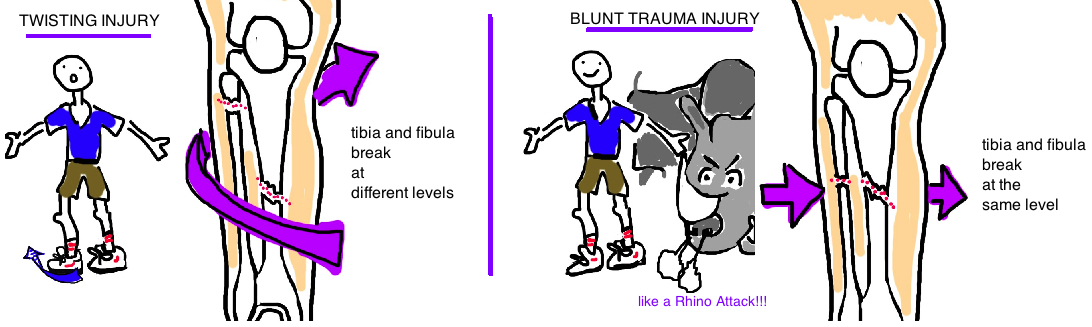
The tibial shaft fracture can occur after a blunt trauma (like in a car accident where the dashboard slams into your shin) or it can occur after a twisting injury (a similar twisting pattern than can also cause ankle fractures). A major issue with tibial shaft fractures is the absence of soft tissue (fat or muscle) covering the bone. Just feel your own shin bone. The bone right there, just under the skin. This means that when the tibia breaks, theres a good chance that a bone fragment will poke through the skin. When the bone goes through the skin, it is called an “open fracture” (or a compound fracture). Open fractures are at increased risk for becoming infected and need to be cleaned in the operating room in a timely manner.
How is a Broken Leg (Tibia Shaft Fracture) diagnosed?
People with a broken leg usually come into the emergency room after an accident unable to put weight on the injured leg due to severe pain. Swelling and pain are common. If bone is exposed through the skin, the diagnose is literally staring you in the face.
An X-ray is ordered and will confirm the diagnosis of a broken leg. X-rays not only give the diagnose but will help to guide treatment. As we will discuss in a minute, a broken leg is treated based on the fracture pattern, not all breaks are the same.
The X-ray will show the number bone fragments, the location of the break, and the pattern of the broken bone. If the break looks complex (lots of pieces, or a break near the knee or ankle joint), then most doctors will order a CAT scan.
A CAT scan is like a few hundred x-rays taken of the leg, in slices...like a loaf of bread. Each slice of bread shows the loaf at a difference section. The same is true of a CAT scan of the tibia bone. The CAT scan helps doctors plan for surgery.
A tibial fracture that occurs in the lower 1/3 of the bone has a high chance (25%) of extending downward into the ankle joint (usually its just a hairline crack). Its important to identify these fracture lines because it affects treatment.
How is a Broken Leg (Tibia Shaft Fracture) treated?
Most broken legs require surgery as treatment.
But not all need surgery! If the broken bone isnt displaced (meaning there is a crack in the bone, but the fragments have not moved out of position) then a long leg cast can be used to protect the bone while it heals (no surgery is needed).
Sometimes, even if the bone fragments have moved, a well molded cast can be applied in a manner that re-aligns the fracture fragments so the bone will heal straight (the bone can actually heal with a little bit of angulation but less than 5 degrees, or a small amount of rotation <10 degrees).
However, the bone fragments need to be in 50% of contact with each other, otherwise there is a low chance the bone will heal. And even if the bone is aligned, usually it takes many months to heal, and that means wearing a big heavy cast for a long time. So many active people will elect for surgery even if alignment isnt an issue.
But more commonly the break is too complicated to heal in the correct alignment by simply treating it with a cast. So how do surgeons repair the broken bone? There are two schools of treatment, both of which use metal to realign the bone.
1) Traditionally these fractures were held in place with a metal plate and screws. An incision was made over the fracture and the plate bridged the fracture site and held the bone in the correct position while the fracture healed. The metal plate itself is not expected to withstand a persons full body weight, rather its function is to hold the bone pieces in position while the body heals. Once the bone heals, people can start walking on the leg again.
2) The other method of realigning the tibia is to insert a thin rod down the center of the bone (our tibia is hollow, and bone marrow lives inside of the thick outer rim). This nail is called an "Intramedullary Nail" (aka IMN). This method is preferred by many surgeons today because the incisions are smaller so the scars are smaller. Only a few small holes are needed to place the rod down the center of the bone, and there is less injury to the soft tissue (fat, skin, muscle) of the leg. This becomes particularly important when there is an open fracture (aka "compound fracture"). In this case, the bone injures the soft tissue when it breaks through the skin. Its best to avoid a double hit to the leg by performing surgery through this area where the tissue is already damaged.
The intramedually nail is very light (made of titanium) and the majority of patients are unable to detect a weight difference between their legs. The rod is held into place by a few screws (technical notes).
Patients are typically allowed to start putting weight onto their leg immediately after surgery (in contrast to a plate, where patients have to wait a few weeks before walking).
When the bone pokes through the skin, the bone and surrounding soft tissue needs to be thoroughly cleaned out within a few hours of the injury to prevent infection. Actually, the most important thing to prevent infection is the time it takes to start antibiotics. Depending on the size of the laceration cause by the broken bone, patients are started on one, two or three antibiotics for 24 to 48 hours after surgery is performed.
What is the long term outcome?
It usually takes a few months (about 4 on average) for this bone to heal.
The outcome from this fracture is generally very good, however there is variability depending on how severe the initial injury was, with particular emphasis placed on the presence of bone protruding through the skin. When the fracture is open, there is a much higher risk for complications, including infection, failure for the bone to heal, and failure of the skin to heal over the bone. Overall, there is no evidence that a plate or a rod (intramedullary nail) is better, and there are pros/cons to both treatment options.
If the bone does not heal, or takes too long to heal, the plate will eventually break from the weight of a persons body (from the repetitive stress put on it by all of the steps we take each day). How does bone withstand the force of our body weight every day...its not stronger than stainless steal, right? Well bone is alive, and unlike steal, it can repair itself from the daily stresses of walking. An inert object like a steal plate will eventually break from the accumulation of small stresses over many weeks. Bone is constantly healing itself and remodeling to withstand these forces.
Knee pain is the most common issues after surgery for this injury. It occurs in almost 50% of people after having an intramedullary nail. This pain can improve after a second surgery to remove the nail.
Reference
1) Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006; 37: 691-97. full article. about 20% open. bimodal distribution-young males, elderly females.
2) Gaston P et al. Fractures of the tibia. Can their outcome be predicted? JBJS Br 1999; 81: 71-76. full article. classification system correlates with time to union etc.
3) Boraiah S et a. High association of posterior malleolus fractures with spiral distal tibial fractures. CORR 2008; 466: 1692-98. full article. distal fx have 25% assoc. posterior mal fx. should get CT scan.
Treatment
2) Bhandari M et al. Surgeons' preference for the operative treatment of fractures of the tibial shaft. An international survey. JBJS 2001; 83: 1746-52. 95% use IMN.
3) Hopper GJ et al. Conservative management or closed nailing for tibial shaft fractures. A randomised prospective trial. JBJS Br 1991; 73: 83-5. full article. IMN dec time to union, rate of malunion, and time off work. displaced tibial fx should get IMN.
4) Karladani AH et al. Displaced tibial shaft fractures: a prospective randomized study of closed intramedullary nailing versus cast treatment in 53 patients. Act Ortho Scand 2000; 71: 160-7. full article. imn vs. cast, 14/27 in cast req. re-reduction, had higher delayed union, malunion, lower outcome scores
5) Court-Brown CM et al. Reamed intramedullary tibial nailing: an overview and analysis of 1006 cases. JOT 2004; 18: 96-101. Nonunion of the diaphysis of long bones. CORR 2005; 431: 50-6. full article. closed fx with imn. infxn: 2%, aseptic nonunion 4.4%. also for nonunions: 90% healed with exchange nailing.
6) Bhandari M et al. Treatment of open fractures of the shaft of the tibia. JBJS Br 2001; 83: 62-8. full article. open fx: infxn is 7% gustilo I, 17% gustilo 3b. nonunion 12% gustilo I, 50% gustilo 3b.
6) Forster MC et al. Should the tibia be reamed when nailing? Injury 2005; 36: 439-44. full article. review of prospective studies, nonunion increased 3x in unreamed fx.
7) Bhandari M et al. Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. JBJS 2008; 90: 2567-78. full article. classic: SPRINT trial: multicenter RCT showed no difference in open fx (29% nonunion reamed, 25% nonunion unreamed). closed fx 10% reamed, 17% unreamed nonunion, but may be from dynamization. showed importance of waited 6 mo before called something nonunion. often takes that long to heal.
8) Van der Linden W, Larsson K. Plate fixation versus conservative treatment of tibial shaft fractures. A randomized trial. JBJS 1979; 61: 873-878. full article. plating is better than nonop, but not good for open fx.
9) Oh CW et al. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. CORR 2003; 408: 286-91. full article. minimally invasive plating good for prox. or distal tibial fx, high union rate, minimize periosteal injury.
Complications
10) Toivanen JA et al. Anterior knee pain after intramedullary nailing of fractures of the tibial shaft. A prospective, randomized study comparing two different nail-insertion techniques. JBJS 2002; 84: 580-5. full article. tendon splitting vs parapatellar approach has no difference, but overall high rate of anterior knee pain (60%).