CHARCOT FOOT
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
related talks: diabetic foot; broken foot (talus fracture, another type); broken foot (jones fracture); broken foot (lisfranc fracture); broken ankle (classic type)
What is a Charcot Foot?
Charcot disease is a progressive condition that destroys the bones and joints of the foot.
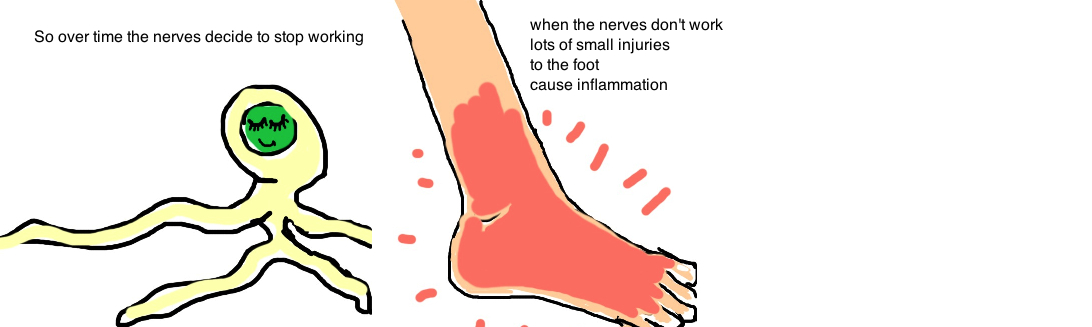
Its a condition most commonly seen in people with diabetes, due to the neuropathy that develops from having too much sugar in the blood. Neuropathy (poor sensation) occurs because, over time, diabetes damages the small sensory nerves in the feet, and this causes people lose the sensation in their feet. This sensory feedback normally provided by these nerves is critical for small adjustments we make subconsciously to rebalance the stresses on our feet while standing or walking. When neuropathy prevents us from making these adjustments, excess pressure builds up in certain areas of the foot, causing stress fractures or joint instability.
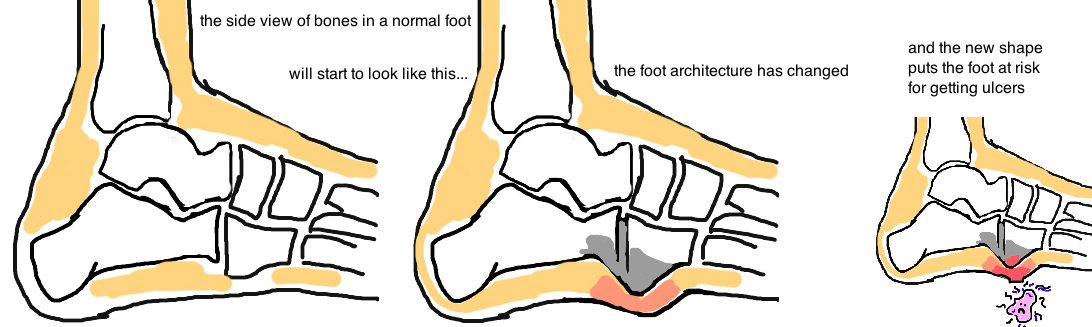
Most people would immediately feel the pain of a stress fracture and would avoid walking on the foot. Yet people with neuropathy cannot feel pain and so they continue to walk on a broken bone. Overtime, repetitive strain will cause permanent structural damage to the feet. This is Charcot. Progressive deformity leads a collapse of the foot arches and further imbalance in weight distribution. It’s a viscious cycle. Eventually ulcers form at the pressure points and the ulcers are at high risk for becoming infected and spreading infection to the bone (called Osteomyelitis).
Another theory of Charcot suggests that diabetes not only injures the nerves but also causes poor blood flow to the feet, leading to unhealthy bones which are more susceptible to the stresses of daily activity and eventually breakdown as a result.
How is Charcot Foot diagnosed?
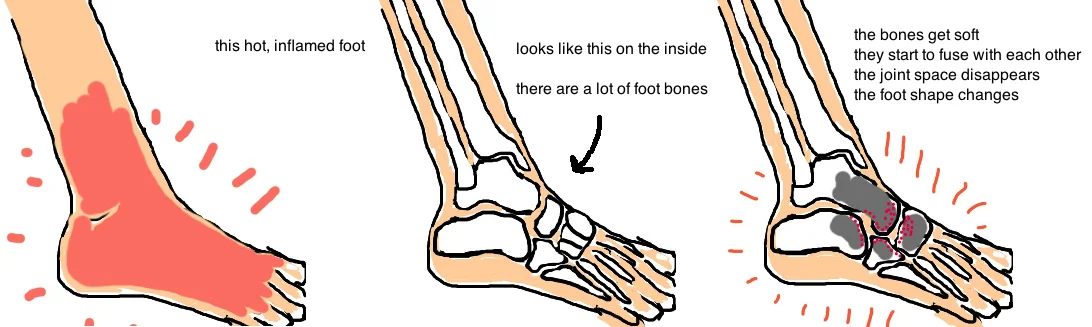
The condition initially presents as a red, hot, and swollen foot.
Its often not painful because the patient has neuropathy and has decreased sensation in their foot. However, neuropathy is a spectrum, not black and white, and so its not uncommon for people to have some degree of pain in the affected foot.
It is important to differentiate (but often very hard to differentiate) this condition from a foot infection, which also has symptoms of redness and swelling. Doctors attempt to differentiate the two by elevating the leg and watching the redness drain out of the foot in Charcot (while it persists in an infection).
Other tests, such as blood tests, MRI scans, or indium scans can provide additional information, but they only provide a general picture of a situation, and can rarely definitively say its one or the other.
X-rays are critical to obtain because they assist in our understanding how far the condition has progressed. After a few months, Charcot will progress beyond the inflammatory phase and enter the fragmentation phase. At this time the X-rays will show bone breakdown, and possible joint dislocations. About 60% of cases involve the midfoot joints (tarsometatarsal joint), while the hindfoot (subtalar) and ankle joint are less commonly involved. Later in the disease process, x-rays will show bone remodeling and healing in their new position.
How is Charcot Foot treated?
The mainstay of treatment is prevention.
Doctors really want to prevent the foot from getting worse. This is accomplished by protecting the foot with casting. The cast will pad pressure points and prevent further bone destruction and ulceration. The cast will also hold the bone and joints of the foot in a stable position while they heal, so that normal alignment is preserved. There is ongoing debate whether patients are allowed to bear weight on the affected leg while the bones are actively inflamed. A big concern of limiting weight bearing on one foot, is that it puts a lot of pressure on the other foot (remember these patients are very susceptible to injury). The flair ups of Charcot (aka the inflammatory phase) will resolve with time, so the focus is on symptom management.
Over the following few weeks or months, as the bones begin to enter the remodeling and healing phase, people are transitioned out of the cast and placed into special braces, and eventually shoes with insoles that improve pressure balance (called a CROW boot, or Charcot Restraint Orthotic Walker).
Sometimes no amount of shoe padding or custom orthotics can accommodate a foot that is very deformed by Charcot. In such cases, surgery can shave down bony pressure points or fuse joints that are unstable to reduce the risk of future ulcerations. Surgery is only recommended once the foot has left the inflammation stage and entered the healing and remodeling phase.
What is the long term outcome?
The Charcot disease will resolve, the bigger concern is the lasting effects of the flair up. Its important to follow the patient with occasional x-rays (to see if the bones are moving out of alignment) and with occasional foot inspections to see if any ulcers are forming. Many patients develop ulcers despite the best efforts of doctors and family. Those which become infected almost always require surgery to wash out the infection.
Overall there is debate about which patients are ideal candidates for surgery and there is no consensus among doctors regarding the best procedures to use.
Reference
1) van der Ven A et al. Charcot neuroarthropathy of the foot and ankle. JAAOS 2009;17:562-71. full article. review.
2) Guyton GP, Saltzman CL. The diabetic foot: Basic mechanism of disease. JBJS 2001; 83: 1083-1096. full article.
3) Feng Y et al. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg 2009;50:675-82. full article.
4) Holmes GB Jr, Hill N: Fractures and dislocations of the foot and ankle in diabetics associated with Charcot joint changes. Foot Ankle Int 1994;15:182-185. full article.
5) Schon LC et al. Charcot neuroarthropathy of the foot and ankle. CORR 1998; 116-131. full article. joints affected, and deformities.
6) Crerand S et al. Diagnosis of osteomyelitis in neuropathic foot ulcers. JBJS Br 1996; 78: 51-55. full article. imaging to diff.dx charcot w. osteomyelitis.
7) Shaw JE et al. The mechanism of plantar unloading in total contact casts: implications for design and clinical use. Foot Ankle Int 1997; 18: 809-817. full article. reduces pressure by 30%.
8) Brodsky JW, Rouse AM. Exostectomy for symptomatic bony prominences in diabetic charcot feet. CORR 1993; 21-26. full article. effective treatment for failed nonop.
9) Cooper PS. Application of external fixation for management of charcot deformities of the foot and ankle. Foot Ankle Clin 2002; 7: 207-254. full article. ring-ex fix good at preventing
10) Dalla PL et al. Use of a retrograde nail for ankle arthrodesis in charcot neuroarthropathy: a limb salvage procedure. Foot Ankle Int 2007; 28: 967-70. full article. 100% limb salvage without major complication.