DIABETIC FOOT ULCER
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
related talks: charcot foot; broken foot (talus fracture, another type); broken foot (jones fracture); broken foot (lisfranc fracture); broken ankle (classic type)
What is a Diabetic Foot Ulcer?
Diabetes is a problem of too much sugar (aka “glucose”). Our intestines absorb the sugar from the foot we eat, the sugar enters our bloodstream, and then the sugar travels in our blood to our muscles and brain to be used as energy. With diabetes our intestines are still able to absorb the sugar, so it enters our blood, but our body is already backed up with too much sugar and our muscles don't want any more to be delivered, so it just sits around inside the blood waiting to be used.
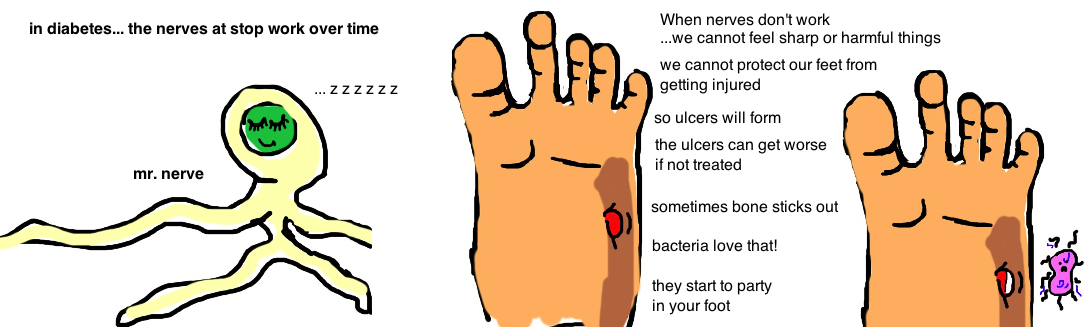
Its a bad thing to have sugar just hanging out in our blood. It is believed that over time diabetes damages the small sensory nerves in the feet, and people lose sensation in their feet (a condition called neuropathy). Sensory feedback from these nerves is critical for small adjustments that we make subconsciously to rebalance the stresses on our feet while standing or walking. When neuropathy prevents us from making these adjustments, excess pressure builds up in certain areas of the foot, causing ulcers to develop. Yet patients don’t even know this is going on because its happening at the bottom of their feet (cannot see the ulcers) and they don’t feel anything (remember they have neuropathy).
The problem is made worse because diabetics also develop artery disease (they have poor circulation) and blood is essential to bringing the necessary nutrients for the body to heal. Because diabetics have poor circulation, these ulcers often heal very slowly, if at all. Sometimes the ulceration goes down to the bone. About 10% of diabetics will develop foot ulcers at some time. Unfortunately, ulcers can become a life threatening condition if not treated carefully, and they are the cause of 85% of foot or below-knee amputations in diabetics.
Here are the keys to prevention and treatment of diabetic ulcers (we will talk more about it below): 1) diagnose the problem: determine if the diabetes is controlled and how bad the neuropathy and circulation to the foot is; 2) regular foot checks to identify ulcers; 3) protect an ulcer by keeping the skin clean and reduce pressure on the area of skin breakdown.
How is Diabetic Foot Disease diagnosed?
The diagnosis is made by examining the foot and looking for skin breakdown ("ulceration"). The severity of the ulcer is measured 0-5 (see picture). A Grade 0 is a foot at risk for developing an ulcer due to an abnormal bony prominence in the foot. A Grade 1 is a superficial ulcer (area of redness) while a Grade 2 is an ulceration of the entire skin thickness. A Grade 3 is like a Grade 2 (complete skin breakdown) plus there is an underlying infection (osteomyelitis or an abscess). A Grade 4 is partial gangrene, meaning the soft tissue is dead and there is an infection. A Grade 5 is extensive gangrene. The presence of an infection is determined in multiple ways, by looking at laboratory information (like WBC count), by looking at the wound itself to see if there is pus or extensive redness around the ulcer, and by asking about recent fevers. Wound cultures are valuable for identifying an infection and determining what type of antibiotics will kill the offending bacteria. MRI scans are often used as well to see if there is an infection in the bone, or an abscess (collection of pus) around a bone.
How is Diabetic Foot Disease treated?
Treatment depends on the severity of the foot ulceration.
A Grade 0 ulcer just requires special shoe wear to prevent progression. A "rocker-bottom" shoe distributes the pressure away from areas of the foot that commonly develop ulcers and effectively reduces the rate.
In a Grade 1, or Grade 2 ulcer people should be fitted with a cast around the foot to take pressure off the ulcer (called total contact casting), which will be worn for up to 4 months to allow time for healing.
However, in a Grade 3, there is an active infection so a cast cannot be used initially. The wound needs to be cleaned (called "irrigation and debridement") in the office or in the operating room. A course of antibiotics are also given. Once the infection appears to be cleared, casting can be used to promote healing.
In a Grade 4, or Grade 5 ulcer, the infection has progressed too far for normal healing to occur, and unfortunately, some type of amputation, to remove the dead tissue and prevent the spread of infection, is typically required.
Treatment is also guided by understanding a persons ability to heal. Blood delivers the immune cells to fight bacteria, and nutrients to allow healing. Diabetes damages small blood vessels and prevents good blood flow to the feet (about 60% of people with diabetic foot ulcerations have some degree of peripheral vascular disease, meaning poor blood flow). The quality of a persons blood flow can be measured by the transcutaneous oxygen pressure (should b e>30 to heal an ulcer) or with ABIs (the ankle-brachial index should be >0.45 to heal an ulcer). The quality of blood flow helps doctors to determine how much of the foot or leg can be saved when a partial amputation is required to remove an aggressive infection that spreads from the ulcer.
What is the long term outcome?
While individual ulcerations can heal with time, diabetic foot disease is unfortunately a problem that typically gets worse if the diabetics continues to cause worsening vascular disease and neuropathy. There is a high risk that recurrence of ulceration will occur.
Reference
1) Wukich DK, Motko J. Safety of total contact casting in high-risk patients with neuropathic foot ulcers. Foot Ankle Int 2004; 25: 556-60. full article. safe and effective.
2) Janisse DJ, Janisse E. Shoe modification and the use of orthoses in the treatment of foot and ankle pathology. JAAOS 2008; 16: 152-8. full article. review.
3) Praet SF, Louwerens JW. The influence of shoe design on plantar pressures in neuropathic feet. Diabetes Care 2003; 26:441-445. full article. rocker shoe best relieves pressure.
4) Pinzur MS et al. Diabetes Committee of American Orthopaedic Foot and Ankle Society. Guidelines for diabetic foot care: recommendations endorsed by the Diabetes Committee of the American Orthopaedic Foot and Ankle Society. Foot Ankle Int 2005; 26: 113-19. full article. recs from major ortho group.
5) Shank CF, Feibel JB. Osteomyelitis in the diabetic foot: diagnosis and management Foot Ankle Clin 2006; 11: 775-89. full article.
6) Robinson AH et al. Surgical aspects of the diabetic foot. JBJS Br 2009; 91: 1-7. full article.
7) Laughlin RT, Chambers RB. Syme amputation in patients with severe diabetes mellitus. Foot Ankle. 1993; 14: 65070. full article. syme amp, ankle disartic w. heel pad coverage has 90% success rx forefoot gangrene if post tib pulse.
8) Lavery LA et al. Probe-to-bone test for diagnosing diabetic foot osteomyelitis: reliable or relic. Diabetes Care 2007; 30: 270-4. full article. probe test 65% accurate dx osteomyelitis, good test, wound cx is very unspecific and not good.
9) Mueller MJ et al. Effect of Achilles tendon lengthening on neuropathic plantar ulcers. A randomized clinical trial. JBJS 2003; 85: 1436-45. full article. all achilles lengthening ulcers healed, dec 2 yr risk by 50%.
10) Maluf S et al. Tendon achilles lengthening for the treatment of neuropathic ulcers causes a temporary reduction forefoot pressure associated with changes in plantar flex power rather than ankle motion during gait. J Biomech 2004; 37: 897-906. full article. temper results of above article b/c weakness persists but pressures return to normal by 8 mo with achilles lengthening.
11) Senneville E et al. Outcome of diabetic foot osteomyelitis treated nonsurgically: A retrospective cohort study. Diabetes Care 2008;31:637-642. full article. nonop rx osteo only 50% heal at 1 yr.