LOW BACK - LUMBAR STENOSIS
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
What is Lumbar Spinal Stenosis?
Lumbar stenosis is a compression of the spinal nerves in the lower back.
As our spinal cord travels down our back, spinal nerves branch off and travel to our arms and legs. The spinal cord travels through the middle of our vertebral bones (in the spinal canal), and then turns into individual spinal nerves at the beginning of our lower back (lumbar spine) called the "cauda equina" (latin for "horses tail" because the collection of nerves looks like a horse tail).
The spinal nerves travel from the spinal canal and pass under the facets (these are tiny joints that connect each of our vertebrae together) this region is called the lateral recess, and finally the nerves exit the spine through a hole between each vertebrae called the "foramen". These spinal nerves can get pinched at any point along this path. Theres barely enough wiggle room for the nerves in a healthy spine, so any narrowing in the path can pinch the nerves causing pain and neurologic symptoms.
Why does the path narrow ?
As we get older our vertebral discs get dehydrated and lose height (this is why people get shorter as they get older). As the disc collapses, it puts more pressure on the vertebral bones (specifically the facet joints) and this causes them to become arthritic and develop bumps called osteophytes. These osteophytes narrow path that the nerve travels along (especially in the lateral recess and the foramen). Loss of disc height alone also narrows the foramen.
Over 80% of lumbar stenosis occurs because of degeneration with age, and symptoms present in our 40s and 50s. The other 20% is associated with spinal abnormalities that people are born with (congenital stenosis), which puts them at much greater risk for developing this disease.
How is Lumbar Spinal Stenosis diagnosed?
Symptoms vary person to person.
About 90% of people with this condition report radicular pain (pain radiating down the leg), and 60% have numbness in their legs, and 40% report weakness in the legs. Pain is usually felt in both legs (but occasionally people report just one leg is affected). The most severe pain is actually in the legs, not in the back, and if back pain is present, its probably related to something else.
People complain of pain when leaning backward (or even standing upright) because this makes the spinal canal and the foramen smaller. In a health spine, leaning backward will narrow the canal by 9%, but in a back with spinal stenosis, simply leaning back will narrow the spinal canal by 66%!
So people feel better when leaning forward...and this is called the "shopping cart phenomenon" because people will develop back pain within 10 minutes of walking around a supermarket, but will then feel great if they leaning forward onto their shopping cart as they continue to shop (it usually provides almost instantaneous relief).
Furthermore, when walking upstairs people with stenosis feel ok (because they bend forward), but when walking downstairs we have to lean backward to keep our center of balance, and this causes pain.
Clogged arteries in the legs (peripheral vascular insufficiency) can also cause leg pain with prolonged walking. Therefore its important for doctors to rule out this vascular condition before diagnosing spinal stenosis.
Images of the spine help with diagnosis. X-rays can be helpful by showing areas of facet arthritis (degeneration in the back of the vertebre bones) and narrowing of the foramen (exiting space for our nerves).
MRIs are probably the most helpful, although they can be overly sensitive. About 20% of people over 60 years old have stenosis of some type seen on MRI, but most people are not complaining of severe back pain. In fact, there is no direct link between the severity of stenosis and the severity of symptoms, so its important for doctors to use information from the symptoms and from the MRI to get a true picture of the condition.
But the MRI is great because it can be used to see exactly which spinal nerves are the source of pain. When an MRI shows nerve compression within the central canal or lateral recess (facet osteophyte) the lower nerve (L5) will be compressed, while narrowing of the foramen will compress the upper nerve (L4).
How is Lumbar Spinal Stenosis treated?
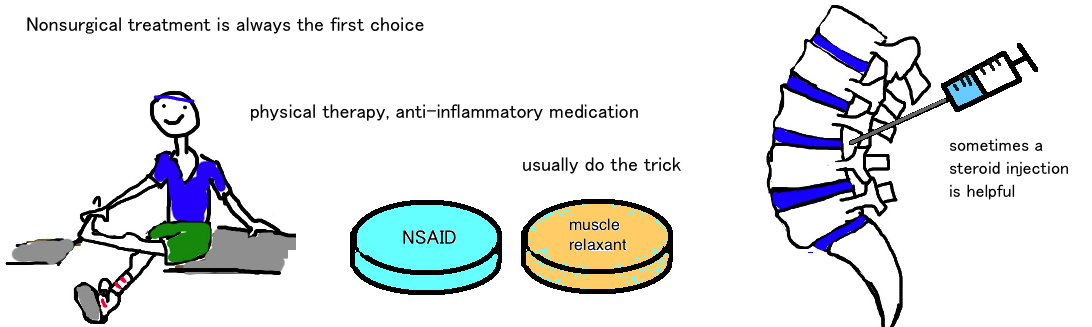
Nonoperative treatment is usually the first treatment. Lumbar stenosis is really arthritis of the spine, a degenerative condition that works slowly, so rapid treatment is rarely required. Therefore its good to try simple, noninvasive treatments first because nothing is lost by trying (except for maybe a few pain weeks). A lot of people will improve with a few weeks of physical therapy.
Epidurals injections also seem to help, with 75% of people reporting at least a 50% improvement in pain, and 60% improvement in walking.
Surgery is considered if 1) nonoperative treatment doesn’t help after a few months, typically doctors wait 3-6 months, or if 2) your nerves continues to worsen and its affecting daily life.
Surgery is most helpful in treating the pain that radiates into the leg, but it helps less with the lower back pain (remember that lower back pain is probably caused by other conditions). Surgery involves a decompression of the spinal canal to give the nerves more breathing room. Sometimes a fusion, combining two or more vertebre, is needed if too much bone needs to be removed to decompress the nerves.
What is the long term outcome?
The patients do well when they are offered the correct treatment based on the severity of their condition.
Overall, surgery tends to help those that dont feel better with nonsurgical treatment. In the short-term (at 2 years) surgery appears to significantly help pain and overall function, however, over time, the benefits of surgery are less apparent to the point that in the long-term, by 8 years, surgery is only a little bit better.
The main reason for “failed” surgery is not really related to the surgery but to the progression of disease. You can treat one region of the spine, but its likely that other regions also have the disease, and can present at any time. Often theres impingement on other nerves and so symptoms return.
Reference
1) Atlas SJ et al. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results form the Maine Lumbar Spine Study. Spine 2005; 30: 936-43. full article. some improved pain with sx, function equal.
2) Weinstein JN et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. NEJM 2008; 358: 794-810. full article. SPORT trial: surgery helps.