BROKEN SHOULDER
(PROXIMAL HUMERUS FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
related talks: shoulder separation (AC joint): broken arm (humeral shaft fracture): shoulder dislocation; broken collar bone (clavicle fracture); shoulder instability (torn labrum)
What is a Broken Shoulder ("Proximal Humerus Fracture")?
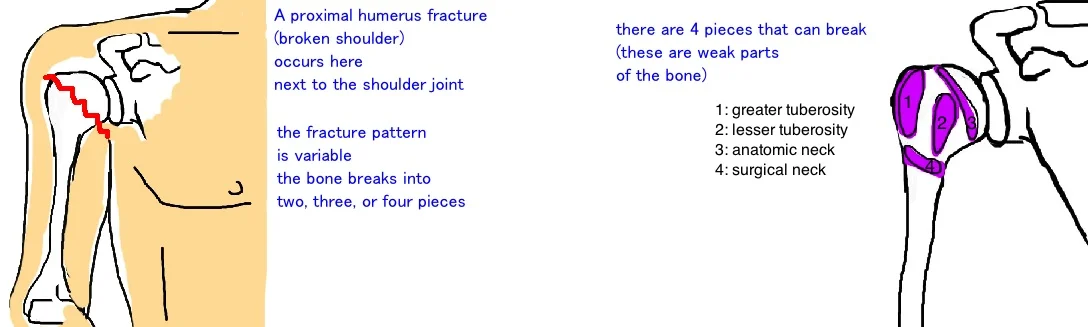
A proximal humerus fracture is sometimes referred to as a a broken shoulder or a broken arm.
This injury occurs right where the arm bone (humerus) connects with the shoulder blade (scapula) to form the shoulder joint. This is why the injury can be called so many things. It involves the arm bone, but occurs at the shoulder joint. So all of these terms are used.
This type of broken bone is most commonly seen in in the elderly population (especially women with osteoporosis), and usually occurs after a fall onto an outstretched arm (people try to brace themselves as they fall). The energy of the fall gets transmitted up the arm, to the shoulder.
How is a Broken Shoulder ("Proximal Humerus Fracture") diagnosed?
A broken shoulder is suspected when someone comes to the doctor complaining of significant shoulder pain after a fall or another traumatic injury. People typically cannot raise their arm due to pain.
The fracture is diagnosed with a series of shoulder x-rays.
The goal of the x-ray is to understand the severity of the break, and also to make sure the shoulder didnt get dislocated. Sometimes the force of the fall can pop the shoulder out of position, and this is a separate issue that usually requires separate treatment (see the talk on shoulder dislocation).
Typically the basic x-rays are all that is required to understand the injury and plan for treatment.
In rare cases where this injury occurs in a younger person, typically after a high speed car accident, then a doctor may order a CAT scan because there are more complex treatment options.
How is a Broken Shoulder ("Proximal Humerus Fracture") treated?
Once diagnosed, the treatment depends on how bad the break is, and also the activity level of the person.
In most of orthopedics there is no universal "Best Treatment" for a given injury. Every treatment option has risks and benefits that need to be tailored to each person's expectations. Its the job of the doctor and patient to talk work together to determine the "Best Treatment" for you as a person.
Now lets take this approach and apply it to proximal humerus fractures.
Doctors grade the severity of this type of fracture based on how many places the arm has been broken, and how far apart the fracture fragments have moved.
There are 4 Parts of the proximal humerus that break, either alone or in combination. 1) The Greater tuberosity; and 2) the Lesser Tuberosity are parts of proximal humerus that can break. They are important because this is where the rotator cuff tendons attach. There is also 3) the Surgical Neck, and 4) the Anatomic Neck of the proximal humerus that can also break.
Now that we understand where the proximal humerus can break, we also need to understand that the broken fragments can move out of position to different degrees of severity. If the fragment breaks, and then moves more than 1 centimeter away from the rest of the bone, doctors consider this displaced. However, if the fragment breaks (has a crack visible on x-ray) but doesn't move out of position, doctors consider this nondisplaced. Fractures that are nondisplaced are expected to heal better than fractures that are displaced. This can influence treatment because doctors are compelled to be more active in assisting the body heal when the fracture is displaced.
The majority of proximal humerus fractures will heal well without surgery. Overall outcome is about the same with or without surgery in most fractures because there is not significant displacement of the bone fragments.
Active range of motion isn’t allowed until bone healing has occurred for 6 weeks. Then you can begin advanced stretching with some early resistance exercise (isometric). Then you move to strengthening (this is done when xrays show the fracture is completely healed), and lastly return to activity-specific exercise.
There are indications for surgery (especially in younger patients because their arm typically breaks only after a high-energy trauma).
If the tuberosities are broken and pulled away too far to heal on their own, then surgery is required. A screw or suture (wire) is used to reattach the broken bone fragment.
If the neck of the humerus is significantly broken, it will also not heal on its own and requires a plate to repair it.
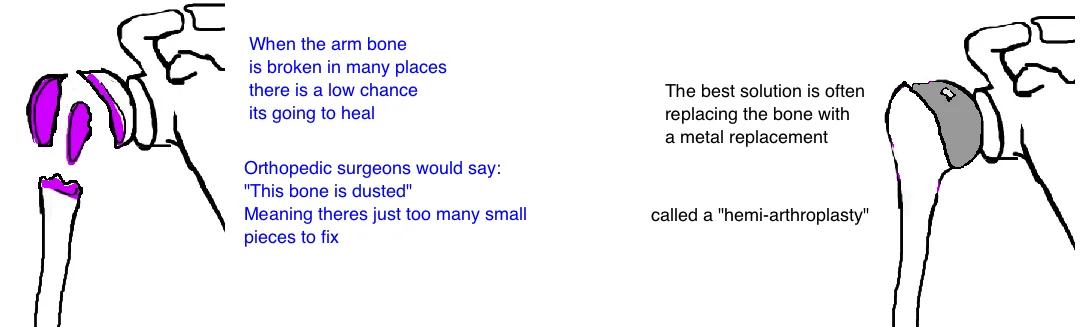
If the head is completely splint, or broken in more than 4 fragments, the bone will probably never heal enough to give you good function. Therefore the best treatment is to replace the bone with a metal head, called a partial joint replacement or a “hemi-arthroplasty”: half of a joint reconstruction.
What is the long term outcome?
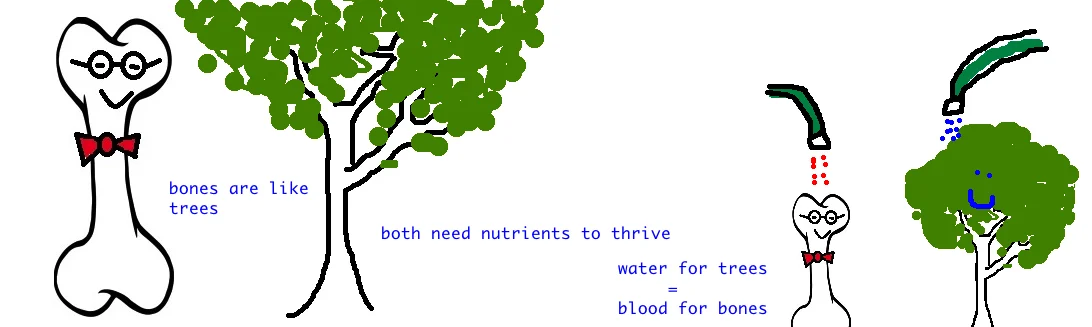
Fractures of the surgical neck, have the highest risk of not completely healing (nonunion: the bones don’t fuse properly) even after a plate is used to stabilize the fracture. This can occur in up to 20% of patients, and is caused by a disruption in the blood supply of the bone (the anterior humeral circumflex artery). See our bone is not like a rock, but more like a tree. It needs nutrients to survive, and in the same way that trees need water, our bones need blood. An injury to the blood vessels at the time of injury to the bone can prevent normal healing.
This complication often requires a second operation, where a blade plate is applied (a different plate which gives more stability) as well as bone grafting (extra bone to stimulate healing), and the vast majority of these patients do very well. After surgery a rehabilitation program is begun immediately with passive range of motion (pendulum and forward flex). If the tuberosity was repaired, the external or internal rotation is limited, depending on which tuberosity was damaged. These fractures are usually treated with a sling and bracing, with rehabilitation and do very well.
Reference
Adult Prox Humerus
Elderly Prox Humerus
1) Bell JE et al. Trends and variation in incidence, surgical treatment, and repeat surgery of proximal humeral fractures in the elderly. JBJS 2011; 93: 121-31. full article. 25% increase in surgical treatment over past decade.
2) Koval KJ et al. Functional outcome after minimally displaced fractures of the proximal part of the humerus. JBJS 1997; 79; 203-7. full article. one pt fx,all healed, 85% good/excellent results, best outcome those starting pt within 14 days.
3) Hanson B et al. Functional outcomes after nonoperative management of fractures of the proximal humerus. J Shoulder Elbow Surg 2009; 18: 612-21. full article. compare injured to noninjured shoulder. constant and dash score worse from 1-part to 2-part to 3-pt fx.
4) Handoll HH et al. Interventions for treating proximal humeral fractures in adults. Cochrane 2012. full article. no best treatment.
5) Maier D et al. Proximal humeral fracture treatment in adults. JBJS 2014; 96: 251-61. full article. review.
6) Iyengar JJ et al. Nonoperative treatment of proximal humerus fractures: a systematic review. JOT 2011; 25: 612-17. full article. nonop rx 3 or 4-part fx high complication rate (50%) - varus (25%)/avn (14%)
7) Hertel R et al. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 2004; 13: 427-33. full article. short metaphyseal extension and disrupted medial hinge increase risk avn.
8) Sudkamp N et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. JBJS 2009; 91; 1320-8. full article. outcome lock plate orif. 33% complication (but 40% were technical error esp. .screw perf). 20% reoperation. but those treated correctly had good Constant scores.
9) Fjalestad T et al. Surgical treatment with an angular stable plate for complex displaced proximal humeral fractures in elderly patients: a randomized controlled trial. JOT 2012; 26: 98-106. full article. older than 60 yo 3 or 4-part orif vs nonop: no difference in outcomes.
10) Olerud P et al. Internal fixation versus nonoperative treatment of displaced 3-part proximal humeral fractures in elderly patients: a randomized controlled trial. J Shoulder Elbow Surg 2011; 20: 747-55. full article. older than 55, 3-part orif vs. nonop: no difference in outcomes (pain, dash, constant, rom),30% reoperation rate.
11) Boons HW et al. Hemiarthroplasty for humeral four-part fractures for patients 65 years and older: a randomized controlled trial. CORR 2012; 470: 3483-91. full article. 4-part fx hemi vs nonop: no difference, hemi complicated by poor greater tub healing.
12) Sebastia-Forcada E et al. Reverse shoulder arthroplasty vs hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder ELbow Surg 2014; 23: 1491-26. full article. R-TSA has better outcomes.